Opioids
York Region is experiencing a drug poisoning emergency like many other regions across Canada. In the past few years, opioid-related deaths have continued to slowly rise.
York Region is responding to this crisis through a number of initiatives, such as:
- York Region Opioid Action Plan
- Community Opioid and Drug Response Collaborative
- Distribution of naloxone kits and harm reduction supplies
- Data and early warning
About opioids
Opioids are substances that can be prescribed to treat pain, severe cough and diarrhea. Some people use opioids because of their euphoric effect. Examples of opioids include fentanyl, heroin, morphine, oxycodone, codeine and hydromorphone. Opioids can be addictive, and if taken at high doses, can cause coma or death. Special types of opioids, including methadone and buprenorphine/naloxone, are used in opioid treatment programs.
What is fentanyl?
Fentanyl is an opioid that is approximately 100 times more potent than morphine and 40 times more potent than heroin. Fentanyl can be prescribed by a physician or obtained through an unregulated, toxic supply. Fentanyl and its analogues are trafficked and sold in many different forms including patch, powder, pill and liquid. “Street” drugs can be contaminated with fentanyl making them more potent and increasing the risk of overdose. Fentanyl use and overdose has been on the rise in Ontario over the last several years.
For more information on opioids, visit Health Canada’s webpage.
Preventing an overdose
Overdose is preventable and so are overdose-related deaths. It’s important to understand the risks and signs as well as the steps you can take to help prevent an overdose in the first place.
What is an overdose?
An overdose occurs when a person uses a drug or combination of drugs that the body cannot handle. The current overdose crisis is largely a result of poisoning from an unpredictable and unregulated supply of drugs. Many overdose deaths are accidental or unintentional.
What are the signs and symptoms of an opioid overdose?
Recognize the signs and symptoms of an overdose, which include:
- Difficulty walking, talking and staying awake
- Blue or purple lips or nails
- Very small pupils (black, circular part of eyes)
- Cold and clammy skin
- Dizziness and confusion
- Extreme drowsiness
- Choking, gurgling or snoring sounds
- Slow, weak or no breathing
- Inability to wake up, even when shaken or shouted at
Call 911 immediately to get help. See the ‘Responding to an opioid overdose’ section below for information about the Good Samaritan Drug Overdose Act.
For more information about opioid overdose, visit Health Canada or Ontario.ca/opioids
Who is at risk of an opioid overdose?
You, your friend or family member is at risk of an opioid overdose if you/they:
- Are taking prescription opioids that were not prescribed to you/them
- Are buying opioids from the street and don’t know how strong they are
- Have bought street drugs contaminated with opioids
- Have overdosed on opioids before
- Are mixing opioids with other downers like alcohol or benzodiazepines (e.g., Valium, Xanax)
- Have stopped using opioids for a while (which lowers tolerance) and start using again
- Are using opioids by yourself
- Are using opioids in a new or different way (e.g., injecting, snorting or crushing)
- Are taking a higher dose than normal
- Are living with or have a history of mental illness (e.g., depression, psychosis)
- Are living with health issues (e.g., liver, kidney, heart, breathing issues)
- Lack sleep (impaired judgment) or food
- Are in a hurry to use
- Have a new dealer or are using unknown substances
How to reduce the risk of an opioid overdose
- Try not to use alone. Make sure someone is around to check on you in case you overdose. If you are alone while using substances, these services below will support you over the phone or call 911, if needed:
- National Overdose Response Service (1-888-688-6677)
- Do not mix drugs or take drugs with alcohol. The risk of overdose increases if opioids are mixed with alcohol, sleeping or anxiety pills, other opioids or other prescription medications
- Try a small amount first. If switching to a stronger opioid, use less and do a test dose
- Start low and go slow. If using opioids after cutting down, or not using for a while, use slowly; don't feel pressured to rush; do a tester dose first to see how you feel
- Check your drug before using. Ask others what they are experiencing with the same batch or if possible, check your drug at a drug checking service in Toronto
- Have and be trained to use naloxone. See the ‘Naloxone and harm reduction supplies’ section below for more information on naloxone
- Create an overdose plan. Talk with your friends and family about overdose and create a realistic plan you can use in the event of an overdose. Make sure they know where you keep your naloxone or ask that they keep their own kit on hand
Responding to an opioid overdose
When you think someone has overdosed, follow the steps below to help save a life.
Always call 911 if someone is overdosing on opioids, whether or not naloxone is used. Naloxone is a non-opioid medication that counteracts the effects of opioid overdose. It comes in a nasal or injectable form.
The Good Samaritan Drug Overdose Act is a federal law that provides legal protection for persons who call 911 to seek medical or law enforcement assistance in a drug overdose situation, whether the person is calling for oneself or another person who is overdosing. The Act provides protections for persons from being criminally charged for simple possession or violation of one’s bail or probation conditions as a result of using drugs, for example. It does NOT provide persons with protection from being charged with more serious offences such as drug trafficking or weapons offences.
Where to get naloxone and harm reduction supplies
Nasal and/or injectable naloxone kits and refills are available without a prescription, at no cost for people who are at risk of opioid overdose and for their concerned friends and family members. Harm reduction supplies include safer injection, inhalation and snorting supplies as approved by the Ontario Harm Reduction Distribution Program. Visit york.ca/harmreduction for more information.
York Region Public Health is currently working with the following partners and others to distribute naloxone and/or harm reduction supplies:
- 360°kids
-
Access York: 24262 Woodbine
-
Access York: 9060 Jane
- Addiction Services Central Ontario
- Blue Door
- Caritas School of Life
- CAYR
- Inn from the Cold
- John Howard Society
- LOFT Street Outreach Van
- Markham Stouffville Hospital
- The Krasman Centre
- The Vitanova Foundation
- York Region Paramedic Services
- York Region Public Health Sexual Health Clinics
Naloxone can also be picked up at a participating pharmacy
If you are a community agency interested in distributing naloxone or harm reduction supplies, please contact the Substance Use Prevention and Harm Reduction Program at 1-877-464-9675 ext. 76683 or @email.
If you are a health professional, visit the following page for Substance Use and Harm Reduction Information.
Support for people who use drugs and their loved ones
Many supports are available to residents who use substances and their loved ones. Click to access a list of Community Services for Alcohol and Drug Use in York Region. The listed community services and supports offer help for individuals experiencing alcohol and other drug concerns. These services are free and confidential (unless otherwise stated).
Opioid trends in York Region
View the latest York Region Opioid Drug Safety Warnings and Bulletins below. If you wish to receive email updates directly, please contact @email to request to add your email to the mailing list.
September 30, 2023
August 4, 2023
June 23, 2023
May 12, 2023
May 5, 2023
March 24, 2023
February 10, 2023
January 4, 2023
October 27, 2022
September 29, 2022
July 28, 2022
July 12, 2022
March 24, 2022
January 20, 2022
December 23, 2021
November 25, 2021
September 9, 2021
August 5, 2021
July 23, 2021
June 11, 2021
April 30, 2021
April 7, 2021
February 5, 2021
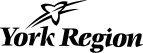
Overall opioid-related harms
Opioid-related harms, including emergency department (ED) visits, hospitalizations, and deaths, have been increasing over the last decade.
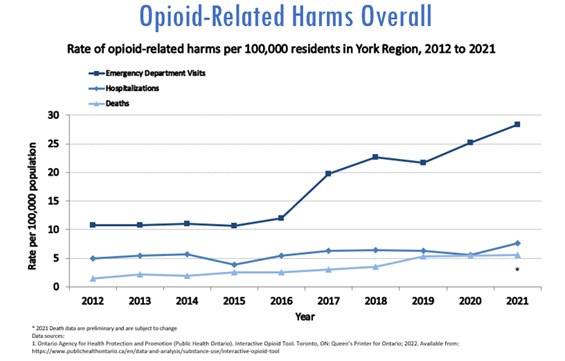
Emergency Department Visits for Opioid Overdoses
York Region Residents
The rate of emergency department visits for opioid overdoses in York Region has slowly increased with a sharper rise in 2017, mirroring the increase in the Ontario rate.
In 2021:
- There were 359 emergency department visits for opioid overdoses in York Region residents (rate of 28.4 per 100,000 residents)1
- 25 to 44 year old males had the highest rate of opioid-related emergency departments visits in York Region1
- Note: Since April 2017, Ontario hospitals have been required to report emergency department visits for opioid overdoses
Hospitalizations for Opioid Overdoses
In 2021:
- There were 97 hospitalizations for opioid overdoses in York Region residents (rate of 7.7 per 100,000 residents)1
- 25 to 44 year old males had the highest rate of opioid-related hospitalizations in York Region1
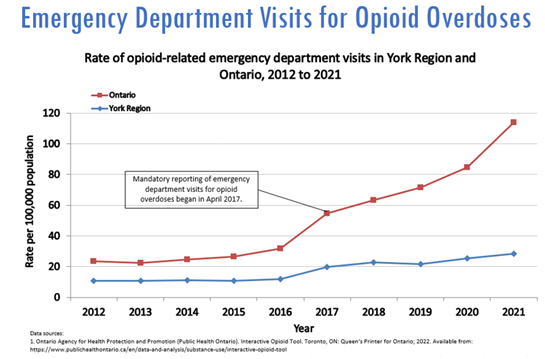
Opioid-Related Deaths
In 2021:
- There were 72 opioid-related deaths in York Region residents (rate of 5.5 per 100,000 residents)1
- 25 to 44 year old males had the highest rate of opioid-related deaths in York Region1
- At time of death, in York Region, fentanyl was present in the vast majority of opioid-related deaths1 **
** Important Note: Death data for 2021 are preliminary and subject to change.
Technical Note: Drug categories are not mutually exclusive meaning there may have been more than one drug present at death.
Technical Notes
- Data last updated on December 16, 2022.
- Population estimates used to calculate emergency department (ED) visits and hospitalization rates are rounded which means there may not be direct comparability to similar calculations.
- There is a significant delay in opioid-related death data.
- There is a slight delay in emergency department (ED) visit data.
- The following ICD-10 codes were used to filter data extraction for ED visits and hospitalizations:
- T40.0 (poisoning by opium), T40.1 (poisoning by heroin), T40.20-T40.28 (poisoning by codeine and derivatives [T40.20], poisoning by morphine [T40.21], poisoning by hydromorphone [T40.22], poisoning by oxycodone [T40.23], poisoning by other opioids not elsewhere classified [T40.28]), T40.3 (poisoning by methadone), T40.40-T40.48 (poisoning by fentanyl and derivatives [T40.40], poisoning by tramadol [T40.41], poisoning by other synthetic narcotics not elsewhere classified [T40.48]), T40.6 (poisoning by other and unspecified narcotics)
- Categories for drug present at time of death are not mutually exclusive.
Source
Ontario Agency for Health Protection and Promotion (Public Health Ontario). Interactive Opioid Tool. Toronto, ON: Queen’s Printer for Ontario; 2021. Available from: https://www.publichealthontario.ca/en/data-and-analysis/substance-use/interactive-opioid-tool
Report bad drugs
Report Bad Drugs (york.ca/reportbaddrugs) is an anonymous online reporting tool for community partners and the public. Anyone with a concern or bad experience with street drugs or overdoses in the community can use the tool to anonymously share information with York Region Public Health.
The information you provide will be reviewed by York Region Public Health staff and used to inform public health actions in the community. The reports are anonymous and no personal or identifying information will be collected. If you have any questions or feedback, please contact the York Region Public Health Substance Use Prevention and Harm Reduction Program at 1-877-464-9675 ext. 76683 or @email
This reporting tool is not for emergencies. If you are experiencing an emergency, call 911 immediately.
York Region Opioid Action Plan
The 2024 Opioid Action Plan builds off the work of the original document launched in 2019, and has outlined 20 different actions, organized into six areas of focus:
-
Stigma reduction
-
Prevention
-
Harm reduction
-
Treatment
-
First response and community safety
-
Data and Early Warning
A community approach is essential. We need to work together to address the challenges faced by our community and people who use drugs.
For more information, please contact the Substance Use Prevention and Harm Reduction Program at 1-877-464-9675 ext. 76683 or email @email
Do Your Part to Reduce Stigma
Whether someone you love or know uses substances or not, you can help reduce the stigma experienced by people who use substances such as opioids. Stigma is negative attitudes, beliefs or behaviours about or towards a group of people because of their situation in life. It includes discrimination, prejudice, judgment and stereotypes, which can isolate people who use drugs and prevent them from talking about their substance use and reaching out for support.
What is stigma?
Stigma is prejudice and discrimination toward people who use substances and/or are impacted by the harms related to substance use. Substance-related stigma originates with or is further perpetuated by intersections of race, colour, socioeconomic status and sexual orientation. Stigma isolates people and can lead to feelings of guilt, shame, hopelessness and greater harm to the individual and community. People can experience stigma as a result of negative language, attitudes or actions towards people who use opioids and other substances.
Stigmatization results in exclusion from activities that are open to others, for example accessing and maintaining work, a safe place to live and other health and social services. The way in which, policies and laws are created can also discriminate against people who use substances. Learn more about the three types of stigma: structural stigma, social stigma and self stigma.
Negative effects of stigma
The negative effects of stigma can include:
- A lack of service options (e.g., safer supply of drugs, supervised consumption and drug checking services) leave people who use drugs vulnerable to poisoning and death
- Criminal penalties for simple possession of drugs for personal use discriminate and disadvantage people, especially people in certain groups (e.g., Black and Indigenous peoples)
- Causing feelings shame and hopelessness
- Believing negative labels make people feel alone and less worthy of respect
- Reduced confidence and lack of hope can impact a person’s ability to get a job, find housing, maintain relationships and ask for help
- Isolation and lack of connection to family, friends and community
- Use of substances alone which increases risk of overdose
- Barriers to accessing health care services, which may result in delayed diagnoses and treatments
- Use of substance as a coping strategy
- Increased risk-taking behaviors
Actions to reduce stigma
Together we can reduce stigma, increase inclusion, empathy and connections by:
- See people for who they are, not for their drug use
- Listen with compassion and respect so people feel heard and understood
- Learn about opioids, addiction and harm reduction
- Talk about stigma and share experiences that impact ourselves or others
- Organize or attend stigma reduction education or community events
- Learn about opioids and how to use naloxone to save a life
- Learn where harm reduction services and supplies are available
- Include people with lived/living experience in stigma reduction work
- Include peer support in health and social services involving substance use
- Review policies and programs to promote equity
- Be inclusive and welcoming to people who use drugs
- Use respectful and non-judgmental language
- Change how we talk about substance use. Use people first language.
- Use “substance use” instead of “drug abuse”
- Use “a person who uses substances” instead of “junkie”
- Use “people living with a substance use disorder” instead of “addict”
York Region joins many groups working to reduce stigma-related substance use. Learn more about stigma, hear personal stories of people affected by the opioid poisoning crisis and how you can create safe and supportive spaces for people who use substances.
Change the language
- Language Matters – Using respectful language in relation to sexual health, substance use, STBBIs and intersecting sources of stigma (Canadian Public Health Association)
- Changing how we talk about substance use (Health Canada)
- Communicating about Substance Use in Compassionate, Safe and Non-Stigmatizing Ways - A Resource for Canadian Health Professional Organizations and their Membership (Public Health Agency of Canada)
- Overcoming Stigma through Language – A Primer (Canadian Centre on Substance Use and Addiction)
Listen
- Beyond Stigma Video Treating Pain in Opioid Use Disorder
- Beyond Stigma Video: Nurturing Circles of Care
- Circles of Care Discussion Guide
- Beyond Stigma Video: Strength in Connection
- Strength in Connection Discussion Guide
- Stop Stigma, Save Lives (Northern Health)
- See beyond – see the lives (Moms Stop the Harm)
- The Opioid Chapters (Ontario Drug Policy Research Network and Healthy Debate: Faces of Healthcare)
- Audio series on opioids: In Plain Sight (Health Canada)
- Voice of harm reduction (Ontario Harm Reduction Network)
Learn
- Reducing Stigma (Towardtheheart.com)
- Overcoming Stigma: Online Learning (Canadian Centre on Substance Use and Addiction)
- Understanding Stigma: A free online course for healthcare providers and other frontline clinicians (Centre for Addiction and Mental health)
- Free online training for healthcare providers to help support people’s mental health (Mental Health Commission of Canada, Centre for Addiction and Mental Health)
- Stigma around Drug Use (Health Canada)
- Stigma + Discrimination (Here to Help)
- Decriminalization for Simple Possession of Illicit Drugs: Exploring Impacts on Public Safety & Policing (Canadian Association of Chiefs of Police)
- Decriminalization: Options and Evidence (Canadian Centre on Substance Use and Addiction)
Act
- Substance Use and the Workplace: Supporting Employers and Employees in the Trades [toolkit] (Canadian Centre on Substance Use and Addiction)
- A Review of Workplace Substance Use Policies in Canada: Strengths, Gaps and Key Considerations (Canadian Centre on Substance Use and Addiction)
- Checklist for Workplace Policies on Substance Use Stigma (Canadian Centre on Substance Use and Addiction)
- A Primer to Reduce Substance Use Stigma in the Canadian Health System (Canadian Centre on Substance Use and Addiction)
- Equity and anti-oppressive approaches (Canadian Substance Use Resource and Knowledge Exchange Centre)
- Each and Every: Businesses for Harm Reduction
International Overdose Awareness Day
On August 31, people across the world take time to bring awareness to drug poisoning (overdose) as well as honour – without judgment or stigma – individuals who have lost their lives because of drug poisoning and acknowledge the grief felt by their family and friends.
We encourage you to use the information on this page to do your part to help end stigma and help prevent drug poisoning-related death.
Visit overdoseday.com to learn more. International Overdose Awareness Day is an initiative of Penington Institute.

Related Resources
- Substance Use and Harm Reduction Information for Health Professionals
- Opioid Overdose Resource during COVID-19
- Substance Use Resources
- York Region Harm Reduction and Needle Exchange Services
- york.ca/reportbaddrugs
- Report Bad Drugs Tool Q&A
- Good Samaritan Resource
- 8 Safety Tips for Substance Use - Postcard