Breastfeeding Information and Support
*The terms breast milk/breastfed/breastfeeding are widely used, but human milk/chestfed/chestfeeding can be used interchangeably. The terms parent/parents are meant to be inclusive of all parents, caregivers, and significant others. We are in the process of reviewing and revising our written materials to be inclusive of all families in York Region.
Human milk is the ideal nutrition for babies and young children. It is the only source of food growing babies need for the first six months of life. Once solid foods are introduced at about six months, human milk continues to be an important source of nutrition for babies and young children. Breastfeeding protects the health of both the baby and the breastfeeding parent and is beneficial for communities.
Breastmilk is safe, clean and contains antibodies which protect against childhood illnesses.
There are many protective factors of breastfeeding. The Public Health Agency of Canada notes that breastfeeding protects a child’s health. Breastfeeding supports cognitive development and decreases a child’s risk of:
- Sudden infant death syndrome (SIDS)
- Diarrhea
- Ear and lung infections
Individuals who breastfeed also benefit from protective factors that increase over time, and are less likely to experience the following the longer they breastfeed:
- Breast and ovarian cancer
- Type 2 Diabetes
- Heart Disease
Breastmilk is cost-effective, protects the environment, and is always available.
York Region, the Public Health Agency of Canada, and Health Canada recommend that children receive exclusive breastmilk for the first six months of their lives. At six months, children can begin to eat age appropriate solid foods. Breastfeeding should continue, along with solid foods, for at least two years to give children the healthiest possible start in life.
You can get an early start by learning about breastfeeding from your doctor, midwife, or public health nurse during the prenatal stage. Prenatal classes can also help you prepare for the arrival of your baby by learning where to get answers about breastfeeding in your community.
Breastfeeding Information and Support
Before Baby Arrives
Many parents make the decision on how they will feed their baby long before the baby arrives. It is important to discuss this decision with your health care provider and share your thoughts and feelings with your parenting partner(s) and supports.
Making breastmilk is a natural process that starts before your baby is born. There are very few parents that cannot breastfeed or make enough breastmilk, especially with early support. Most parents who have medical conditions or diseases or are taking medications can breastfeed. Only a very small number of parents should not or cannot breastfeed. Talk to your health care provider and call York Region Health Connection for more information on how to maximize your milk supply and support feeding your baby safely.
During pregnancy your body and your baby are getting ready to breastfeed:
- Your breasts may get larger and may feel heavier or tingly as they get ready to produce milk
- Your nipples and areolas (the tissue around your nipples) will get darker and may get larger
- Your baby will practice sucking and swallowing
- Your breasts will be making colostrum during your second trimester. You may even notice your breasts leak long before the baby is born
- Colostrum is the first milk, is yellow-ish and thick and is very important to your baby. It provides your baby with all the nutrition and fluid needed in the first few days of life and strengthens your baby’s immune system
It is rare that individuals cannot produce enough breastmilk. Parents who have experienced the following are encouraged to speak to their health care provider to discuss how this may impact your breastfeeding/chest feeding goals:
- Infertility or difficulty getting pregnant (including polycystic ovarian syndrome)
- Obesity
- History of low milk supply
- Differences in breast size/shape
- Diabetes (if not well controlled)
- Thyroid issues (hypothyroidism)
- Breast reduction or other surgeries
- Receiving gender affirming hormones or surgeries to the chest tissue (chest masculinization surgeries, “top surgery”)
- Minimal or no change in breast size or appearance during puberty or pregnancy
Even with these conditions, most individuals can produce all or most of the milk their baby needs. While exclusive breastfeeding is recommended, any amount of breastmilk is beneficial for your baby.
It is also very possible to breastfeed twins, triplets or more! Here are some helpful tips for Breastfeeding Multiples.
Learning about breastfeeding during pregnancy is a great way to be prepared for feeding your baby after delivery. York Region offers an online prenatal program which provide valuable information about getting breastfeeding off to a great start, in addition to prenatal video consultations with a Public Health Nurse. Contact York Region Health Connection for more information.
Hand Expression
Hand expression in the first hour after birth and continuing after each feeding helps to establish a good milk supply, even when breastfeeding is going well.
Early and frequent hand expression is important to be able to provide milk for your baby and can help establish your milk supply.
Hand expression can:
- Provide your baby with a taste of milk to get them interested in feeding
- Soften the area of the breast surrounding the nipple (areola)
- Lessen the discomfort of overfull breasts
- Help maintain your milk supply if you are separated from your baby or unable to feed your baby directly from the breast
- Save the cost of a breast pump
It is normal to get very little or no milk at first. You may only get a few drops or a teaspoon initially. This is the perfect amount for your new baby’s small tummy in those first few days. The more you hand express over time, the easier it will become and the more milk you will get.
York Region provides Hand Expression Kits at no cost to help support learning how to hand express. Ask your hospital nurse for your free kit.
[IMAGE]
Resources
The First 72 Hours
To help get breastfeeding off to a good start, try:
- Leaning back and put baby skin-to-skin vertically on your chest
- Allow and assist your baby to crawl toward your breast (Baby-Led Latching)
- Breastfeed your baby within the first hour after birth
- Get help right away if your baby is not showing interest in latching to the breast by calling Health Connection at 1-800-361-5653 or visiting york.ca/NurseChat to request virtual breastfeeding support
- Offer your breast every two hours or sooner when baby is showing signs of hunger
Skin-to-Skin Contact is Important
Skin-to-skin contact within the first hour after birth is important to help get breastfeeding off to a great start. You can cuddle skin-to-skin with your baby as soon as possible after birth and between feedings. Spending time skin-to-skin will help your baby:
- Stay warm
- Recover from birth
- Follow the instinct to latch and feed at the breast
Getting a Good Latch at Every Feeding is Important
To encourage a good latch, you can:
- Wait until the baby moves toward your breast
- Align your nipple to your baby's upper lip and wait for your baby to latch
- Support your breast while your baby latches and feeds
- Make sure that your baby feels supported and comfortable
Some babies latch better when the breast is shaped into a “sandwich”. To do this, sandwich the breast tissue in the same direction of your baby’s mouth to make it smaller and easier to grasp.
When your baby is latched well:
- Your baby's chin and cheeks should be touching the breast and head tilted back slightly
- Their nose will be tilted away from the breast
- Their mouth will be open wide, and their lips are flared
- Their chin and lower lip will touch the breast first
- They will have more of the breast below the nipple in their mouth
- They will have a strong and regular suck
- You will hear your baby make a "kaa" sound when swallowing. These swallows become more frequent each day. By day three or four you will hear a swallow for every one or two sucks
If your baby is latched well, it is unlikely to cause pain or damage to your nipples. If you are experiencing discomfort during breastfeeding that does not improve, seek our support by calling York Region Health Connection to speak with a public health nurse for support.
Try Different Positions
It is important that both you and your and baby feel supported and comfortable while breastfeeding. A public health nurse or breastfeeding clinic can help you find positions that work best.
When in a good position for breastfeeding:
- You will not experience pain or discomfort
- Your back will be well supported
- Your baby’s nose will be lined up with your nipple to latch (nose to nipple)
- The baby’s tummy will be facing your tummy
- You can hold your baby close to your body, without gaps between you and your baby (such as blankets, pillows, etc.).
- Your baby’s neck, shoulders and bottom will be supported
Day Three Onwards
Breastmilk production works by supply and demand. The more often your baby breastfeeds and successfully removes milk from the breast, the more breastmilk is made. Breastfeed your baby at least eight times every 24 hours to ensure you produce enough milk to feed your baby.
Breastmilk will start to change 72 hours after birth:
- Breastmilk volume will begin to increase, and your breasts may feel full and warm
- Breastmilk will gradually change from sticky yellow colostrum to white, mature breastmilk over the first two weeks
Remove your breastmilk frequently by hand expression or double electric pump if your baby is not able to breastfeed. Removing milk at every 2-3 hours will help protect your supply. A public health nurse can help answer your questions about which method is recommended for you.
When to Switch Breasts
- Keep the baby on the first breast as long as the baby is swallowing milk frequently
- Offer the second breast when the first breast feels softer or when there are less swallows
- Offer both breasts again if the baby is still showing signs of hunger after feeding at both breasts
By the end of the feed at least one breast should feel soft, and your baby should no longer be showing signs of hunger
What To Do If Your Breasts Are Sore and Hard
Hard, sore breasts can be treated by placing a cold compress or ice pack on your breasts to reduce swelling between feedings. If your baby cannot latch because breasts are too full and hard, remove some milk by hand or with a pump first. This will soften the nipple/areola area to allow your baby to latch. You can also try Reverse Pressure Softening.
Tips for When Baby is Not Latching Well
If your baby is not latching well, try:
- Being patient and don’t give up; it may take days or weeks for the effects of birth to wear off
- Hold your baby wearing only a diaper skin-to-skin (this helps your baby recover from birth and encourages feeding)
- Feed your baby another way while they continue to work on breastfeeding
- Continue to remove milk from your breasts every 2-3 hours by hand expression or with a breast pump
- Breastfeed or express breastmilk about eight times every 24 hours to keep breastmilk production up
- Get help; a health care professional or breastfeeding clinic can support parents through this time and provide expert breastfeeding help
Signs of Hunger
Feed your baby at least eight times every 24 hours. Your baby will show you when they are ready to eat with the following early hunger cues:
- Wiggling, tossing, and turning or restlessness while sleeping
- Moving their hand towards the mouth and sucking on their fists
- Licking their lips
- Making sucking motions or sounds
- Rooting (opening their mouth, searching to suck, and sucking on contact)
- Turning their head back and forth
- Sticking out their tongue
- Making soft cooing or sighing sounds
- Moving their arms and legs
Try to feed your baby when you see these early signs and not later when they are already crying. Crying is a late sign of hunger. If your baby is too upset to breastfeed well or latch, you can try:
- Sitting your baby upright on your chest, skin-to-skin
- Talking, rocking, or gently stroking your baby in a calming way
- Feeding your baby a small amount then trying again at your breast
Feed Your Baby Frequently
In the first six months, most babies will need to breastfeed at least eight times every 24-hours based on their feeding cues. It is normal for babies to breastfeed 12 or more times in a 24-hour period. Babies may cluster some feedings together and then leave longer periods between other feedings. It is important to follow your baby’s cues for feeding.
During the first several weeks of life, your baby may want to feed many times during the night. It may seem that they have “night and day mixed up”. This is normal for newborn babies.
As your baby gets older, they may have longer stretches between feeds. Always follow their cues. Cue-based feeding will help your baby grow and gain weight and will increase your milk production to match your baby’s needs.
If your baby is not waking up to feed, speak to your healthcare provider.
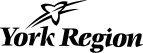
Wet and Dirty Diapers
Diapers are the best way to tell if your baby is getting enough milk.
If your baby is not making enough wet or dirty diapers or the stool is still dark after day four, speak with your health care provider and seek breastfeeding support.
Day One
- One wet diaper
- One black or dark green stool
Day Two
- Two wet diapers
- One or two black or dark green stools
Day Three
- Three wet diapers
- At least two to three brown, green or yellow stools
Day Four
- Four heavy wet diapers
- At least three brown, green, or yellow stools
Day Five
- Five heavy wet diapers
- At least three large, soft yellow stools
Day Six and On
- Six heavy wet diapers
- At least three large, soft yellow stools which may be runny and seedy
Breastmilk Alternatives
Just Breastmilk for Six Months
Your baby does not need any foods or drinks other than breastmilk until six months of age. They can then be given solid foods, along with breastmilk. It is recommended babies continue to breastfeed with solid foods for at least two years. Breastmilk continues to provide older babies and toddlers with protection against illness and disease and continues to be an excellent source of nutrients for young children.
There is no need to give your baby water in the first six months of life — breastmilk has all the water babies need. Giving additional water to your baby in the first six months is not recommended.
All babies need vitamin D. Vitamin D has already been added to infant formula, however, breastfed babies and babies receiving breastmilk will need 400IU of vitamin D supplement each day. Talk to your health care professional about giving vitamin D to your baby.
Supplementing with Infant Formula
Supplementing with infant formula when not necessary can impact breastfeeding and your baby’s health. Talk to a health care provider, public health nurse or breastfeeding expert about how and when to give extra milk, also known as supplementing. Most breastfed babies do not need supplements. Babies may need supplements if:
- They are not having enough wet and dirty diapers for their age
- A health professional is worried that your baby is not growing well
- They cannot latch at the breast or do not drink well at the breast
- A health professional has assessed that breastmilk supply is low
- There is not enough expressed breastmilk available
- You have been separated from your baby for medical or other reasons
If you think your baby needs extra milk, talk to a breastfeeding expert as soon as possible for help. Getting help as early as possible with breastfeeding can help avoid the need for supplementation with extra milk.
If Supplements are Needed
Still try to give as much breastmilk as possible if supplements are needed. Breastmilk can be removed by hand expression or using an electric pump. This milk can then be fed to your baby. If your baby is hospitalized and needs extra milk, ask the hospital staff if pasteurized human milk from an accredited milk bank is an option.
For a step-by-step guide to hand expression of breastmilk, see the Hand Expression factsheet.
To watch a video which demonstrates hand expression, visit: Hand Expression Video - Stanford University
For information on how to safely store and use expressed breastmilk, see Storing expressed breastmilk factsheet.
Infant formula can be used if sufficient breastmilk supply is not produced. Talk to a healthcare provider about what kind of infant formula to provide if your baby needs extra milk and read our infant formula factsheet for information and safe preparation and storage instructions. Unless otherwise advised by your health care provider, commercial cow’s milk infant formula approved for use in Canada is the only acceptable alternative to human milk. Homemade formulas are NOT a safe alternative.
There have been supply shortages for certain infant formulas. For more information, please visit Health Canada.
Making an Informed Decision About Artificial Nipples and Pacifiers
Offering an artificial nipple or pacifier/soother may lead to feeding cues being missed. It is important that you can read your baby’s cues to know when they are hungry versus when they are full.
If babies need extra milk, you can try an alternative feeding device such as:
- Tube at the breast
- Finger-feeding tube
- Cup
- Spoon
For information about the use of any of the above feeding methods, please see the When your breastfed baby needs extra milk booklet.
To help calm your baby, try cuddling, rocking, and placing your baby skin-to-skin.
Breastfeeding Support Options
If you need help with breastfeeding, you can get support:
- Contacting Health Connection at 1-800-361-5653 or through Live Chat
- At one of York Region’s Breastfeeding Clinics
- Calling Health 8-1-1 (24-hour support)
- Contacting La Leche League Canada at 416-483-3368
Seek help if:
- Your baby is not having enough wet or dirty diapers
- Your baby is not able to latch or cannot latch well
- Your baby still seems hungry after breastfeeding and you have to feed your baby extra milk. Read our When your Breastfed Baby Needs Extra Milk factsheet for more information
- Your baby does not regain their birth weight after 14 days
- A health professional is worried about your baby’s growth
- You have sore nipples or breasts
- You have questions or want information or advice about feeding your baby
Breastfeeding and Returning to Work or School
Continued breastfeeding into toddlerhood after returning to work or school is possible and can often be incorporated into a family’s daily routine. Continued breastfeeding is important to the health of both you and your baby, and is a protected right covered under The Ontario Human Rights Commission.
Why Continue Breastfeeding?
Health Canada, the World Health Organization, and the Canadian Pediatric Society recommend that babies be fed only breastmilk for the first six months (exclusive breastfeeding). When your baby is showing signs of readiness for solid foods at around six months, it is recommended to introduce solid foods and continue breastfeeding for two years or longer.
Breastfeeding protects the health of both the child and breastfeeding individual. Many of the protective effects of breastfeeding increase over time. The longer a child is breastfed or receives human milk, the greater the protective health effect.
Breastmilk:
- Helps to protect a child from common childhood illnesses, such as ear and lung infections, as well as diarrhea
- Decreases a child’s risk of sudden infant death syndrome (SIDS)
- Supports a child’s immune system. Some of the illness-fighting cells present in breastmilk increase during the second year of lactation. This makes breastfeeding two years and beyond important to a toddler’s health
- Continues to be a valuable source of nutrition for children, well beyond one year of age. Necessary vitamins, minerals and energy continue to be supportive of healthy growth and development
- Is important to the breastfeeding individual’s health. Individuals who are breastfeeding or expressing milk have a decreased risk of breast and ovarian cancers and heart disease
Did You Know?
Individuals who breastfeed after returning to work take less time off work to care for ill children. This is because breastfed children get sick less often.
What Are the Options for Continued Breastfeeding?
There are several ways to continue breastfeeding or providing expressed breastmilk after returning to work or school.
Options include:
- Having someone bring your child to work or school to be breastfed. Employers and schools will accommodate this as breastfeeding is a protected human right
- Expressing breastmilk at work or school and storing it in a fridge or insulated cooler with ice pack. Expressed breastmilk can then be fed to your child in your absence
- Breastfeeding before leaving for work or school, when you get home, and before bedtime. Milk supply will adjust to meet the needs of your child. However, once breastmilk supply has decreased, it may be difficult to increase again later
What Are My Rights?
The Ontario Human Rights Commission states that you have the right to breastfeed your child or to express your breastmilk, while at work or school. To learn more about this human right, please visit www.ohrc.on.ca
Your Employer Must:
- Protect and support your right to breastfeed and express your milk
- Allow enough time to breastfeed or express milk during your work hours. This time is not counted as break time. You are not expected to miss regular meal breaks or work additional time to make up for time taken to breastfeed or express milk
- Provide a clean and private space for you to breastfeed or express milk
Tips For Returning to Work or School:
Before you return:
- Talk to your employer or school administrator about your plans to breastfeed or express your breastmilk
- Talk to other breastfeeding individuals who spend time away from their children
- Practice expressing breastmilk by hand or pump
- Buy an insulated cooler bag to store breastmilk or ensure there is a fridge at work or school that you can use to store your expressed milk
- Review Storing Expressed Breastmilk
While you are at work or school:
- Wear a supportive and comfortable bra
- Express your milk when you feel full or uncomfortable, approximately every three to five hours depending upon the age of your child
- Expect that it may take days or weeks for your breastmilk supply to adjust to the amount of milk being removed
What Will Be Helpful for My Child?
- Breastfeed right before you leave the house and when you return home. Your child may wish to breastfeed frequently during the evening or before bedtime.
- Understand that it is not unusual for children to want to breastfeed more often at night once separated from their parents in the day. This may be short term, as your child adjusts to a new routine.
- Breastfeed following cues when you are with your child
- If you will not be directly breastfeeding your child at school or in the workplace, have your child practice drinking in another way. Have your child practice drinking from an open cup. While spill-free cups are an option, practicing drinking from an open cup is an important feeding skill for them to learn.
- By 18 months, children should be breastfeeding and/or drinking from a cup without a lid or open cup. Using a bottle should stop by eighteen months, as prolonged use may lead to dental problems
How Can My Childcare Provider Support Breastfeeding?
Choose a childcare provider who:
- Understands that breastfeeding is important to health
- Will support your feeding goals and welcomes you to breastfeed during drop off and pickup
- Accepts expressed breastmilk to feed your child in your absence
- Has a policy about how to store and offer expressed breastmilk
Remember, breastfeeding and expressing breastmilk at work, school or in public is a human right in Ontario. You have the right to breastfeeding anywhere, anytime!
Becoming a Breastfeeding-Friendly Place
The Ontario Human Rights Code says women have the right to breastfeed, undisturbed in any public place in Ontario without being asked to cover up or move to a more discreet area.
The Becoming a Breastfeeding-Friendly Place guide provides businesses and public establishments with step-by-step instructions and resources to create breastfeeding-friendly and welcoming spaces. Decals are available for display in your establishment to promote breastfeeding in public and to attract families to your organization. Call Access York at 1-877-464-9675 to request yours today!
By welcoming breastfeeding families, your business will:
- Publicly acknowledge the rights of breastfeeding families
- Attract families to your facilities
- Align your organization with the promotion of health and wellness
By supporting and welcoming breastfeeding families, you are joining many other businesses and organizations that are committed to promoting a healthy community.
Breast Pump Discretionary Benefit Program
If you receive Ontario Works (OW) or Ontario Disability Support Program (ODSP) benefits you may be eligible to receive funding to rent or purchase a breast pump, if needed.
A breast pump may be helpful for the following reasons:
- To provide breast milk/human milk* for your baby if you are separated
- To keep up your breastmilk production during routine separations (shared custody, work, school)
- To help increase milk production if needed
- If your baby is not able to breastfeed well, or if your baby was born prematurely
See the Breast Pump Discretionary Fund Client Information Sheet to learn more.
More Information
To speak with a public health nurse about breastfeeding and to find out where to get help in York Region, contact:
Health Connection
Telephone: 1-800-361-5653
Email: @email